Scarlett Lin Gomez, PhD, Director, Greater Bay Area Cancer Registry, Cancer Prevention Institution of California (NAACCR Member)
Asian Americans are generally considered as one racial/ethnic group in federal, state, and local health statistics. Until recently, they have been lumped together with the Native Hawaiian and Pacific Islander classifications as one “Asian/Pacific Islander” category. In fact, the Asian American category is heterogeneous, comprising populations from nearly 30 countries, and differing widely in migration patterns, socioeconomic status, health behaviors, and culture, all of which contribute to differences in disease incidence. An increasing number of reports and publications of late have documented differences in risk factors and disease outcomes among distinct ethnic groups when the data are disaggregated. Cancer incidence is no exception, with thanks to the long legacy and commitment within the US cancer registries to collect detailed Asian American race/ethnicity data, we have been able to document cancer patterns for distinct ethnic groups, finding important differences to inform clinical, public health, and policy efforts.
We recently leveraged 26 years of data from the California Cancer Registry, which covers the state with the largest Asian American population in the US, to investigate breast cancer incidence trends among seven Asian American ethnic groups. Our findings included: continuing increases in rates of breast cancer among women from all seven Asian American ethnic groups, with the largest increases for South Asians, Vietnamese, and Southeast Asians – the most recently immigrated groups; rates among Japanese and Filipino women under age 50 comparable to those in non-Hispanic White women; increasing trends over time of distant stage disease, particularly among Filipino, Korean, and South Asian women; and higher rates of some types of HER2-overexpressing tumors among Filipino and Vietnamese women relative to non-Hispanic White women. These patterns warrant additional attention to public health prioritization of disparities in access to care, as well as further research in identifying relevant breast cancer risk factors.
Click here to view the article
Breast Cancer Research and Treatment
Abstract
Purpose: In contrast to other US racial/ethnic groups, Asian Americans (AA) have experienced steadily increasing breast cancer rates in recent decades. To better understand potential contributors to this increase, we examined incidence trends by age and stage among women from seven AA ethnic groups in California from 1988 to 2013, and incidence patterns by subtype
Methods: Joinpoint regression was applied to California Cancer Registry data to calculate annual percentage change (APC) for incidence trends. Incidence rate ratios were used to compare rates for AA ethnic groups relative to nonHispanic whites (NHW).
Results: All AA groups except Japanese experienced incidence increases, with the largest among Koreans in 1988–2006 (APC 4.7, 95% CI 3.8, 5.7) and Southeast Asians in 1988–2013 (APC 2.5, 95% CI 0.8, 4.2). Among women younger than age 50, large increases occurred for Vietnamese and other Southeast Asians; among women over age 50, increasing trends occurred in all AA ethnic groups. Rates increased for distant-stage disease among Filipinas (2.2% per year, 95% CI 0.4, 3.9). Compared to NHW, Filipinas and older Vietnamese had higher incidence rates of some HER2? subtypes
Conclusions: Breast cancer incidence rates have risen rapidly among California AA, with the greatest increases in Koreans and Southeast Asians. Culturally tailored efforts to increase awareness of and attention to breast cancer risk factors are needed. Given the relatively higher rates of HER2-overexpressing subtypes in some AA ethnicities, research including these groups and their potentially unique exposures may help elucidate disease etiology.
The opinions expressed in this article are those of the authors and may not represent the official positions of NAACCR.




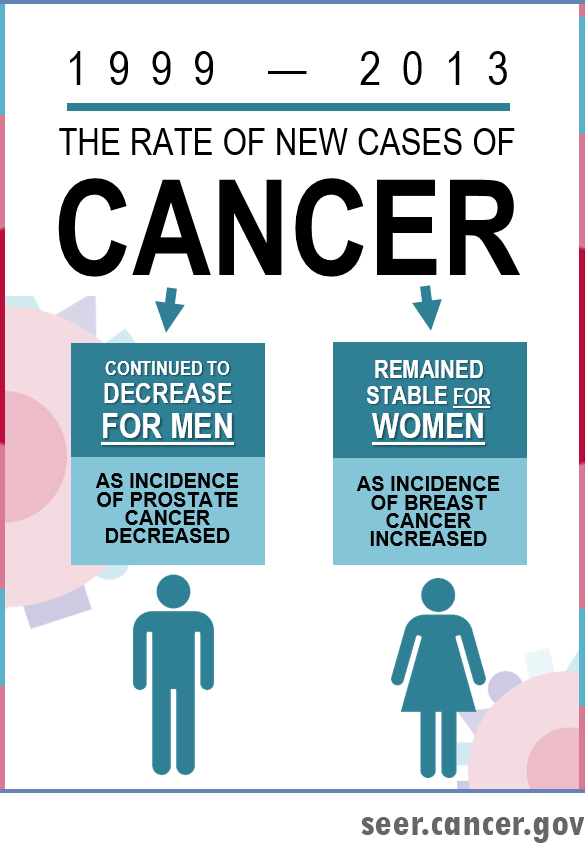 During 1999-2013, the overall cancer incidence rates continued to decrease among men and remained stable among women. The overall cancer death rates continued to decline during 2000-2014 among men, women, and children. The decreases in death rates are the continuation of trends over the past 20 years. Factors that have contributed to these decreasing trends include reduced tobacco use, improved early detection (e.g., colorectal, breast, and cervical cancer), and improved treatments for many cancers. In particular, due to public health policies against tobacco and increased awareness of the health hazards of smoking, adult smoking prevalence has decreased by over 50% over the past five decades. However, tobacco use still accounts for nearly one-third of cancer deaths in the U.S. and about 40 million of Americans still smoke. These facts underscore the need for expansion of tobacco control programs and the development of new strategies to accelerate the reduction in tobacco use.
During 1999-2013, the overall cancer incidence rates continued to decrease among men and remained stable among women. The overall cancer death rates continued to decline during 2000-2014 among men, women, and children. The decreases in death rates are the continuation of trends over the past 20 years. Factors that have contributed to these decreasing trends include reduced tobacco use, improved early detection (e.g., colorectal, breast, and cervical cancer), and improved treatments for many cancers. In particular, due to public health policies against tobacco and increased awareness of the health hazards of smoking, adult smoking prevalence has decreased by over 50% over the past five decades. However, tobacco use still accounts for nearly one-third of cancer deaths in the U.S. and about 40 million of Americans still smoke. These facts underscore the need for expansion of tobacco control programs and the development of new strategies to accelerate the reduction in tobacco use.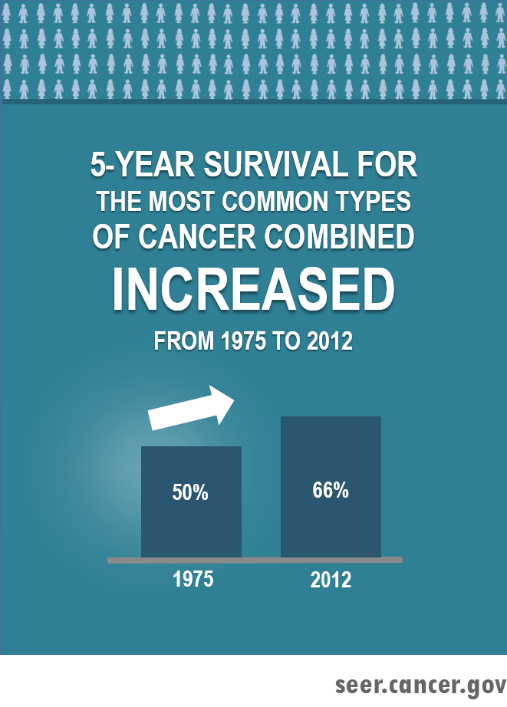 This year’s ARN features cancer survival. Reflected by a 16% absolute increase in 5-year relative survival from 1975-1977 to 2006-2012 for all cancers combined, the overall cancer survival has been improving over the past four decades. By cancer site, the greatest absolute increases in survival rate were found for cancers of the prostate, kidney, NHL, myeloma, and leukemia. Both advances in treatment and declines in surgical mortality may have contributed to the improvements in survival. However, no improvements in survival have been found for cancers of the cervix and uterus. Five-year relative survival remained low for some cancer sites such as pancreas (8.5%), liver (18.1%), lung (18.7%), and esophagus (20.5%).
This year’s ARN features cancer survival. Reflected by a 16% absolute increase in 5-year relative survival from 1975-1977 to 2006-2012 for all cancers combined, the overall cancer survival has been improving over the past four decades. By cancer site, the greatest absolute increases in survival rate were found for cancers of the prostate, kidney, NHL, myeloma, and leukemia. Both advances in treatment and declines in surgical mortality may have contributed to the improvements in survival. However, no improvements in survival have been found for cancers of the cervix and uterus. Five-year relative survival remained low for some cancer sites such as pancreas (8.5%), liver (18.1%), lung (18.7%), and esophagus (20.5%).