
Zeinab El-Masri
Senior Specialist, Knowledge Dissemination & Evaluation, Surveillance & Cancer Registry
Cancer Care Ontario
The need
An important public health goal is to decrease the prevalence of behavioural risk factors which play a role in the burden of cancer and other chronic diseases.
In Ontario, data on behavioural risk factors are available for large administrative areas from survey data. However, there exists a need for high quality local data to enable public health to better understand heterogeneity in the health of their communities.
A novel solution
Dr. Laura Seliske and Todd Norwood from Cancer Care Ontario collaborated with other cancer surveillance researchers to use advanced spatial analysis methods to produce micro-area estimates of behavioural risk factors from existing survey data. The survey methods are similar to the Behavioural Risk Factor Surveillance System in the U.S. The micro-areas selected, census dissemination areas (DAs), are the smallest geographic unit for which complete census data are available in Canada, with average populations of 400 to 700 people.
In their study, a spatial Bayesian hierarchical model was used to estimate the micro-area prevalence of current smoking and excess body weight within one region in Ontario, allowing the researchers to detect areas, or neighbourhoods, of higher prevalence. The abstract and link to the full manuscript can be found below.
 Producing an atlas
Producing an atlas
These advanced statistical methods were adopted to model small-area risk factor prevalence across all of Ontario to produce an atlas—the first of its kind in Canada—with more than 300 maps. Cancer Risk Factors Atlas of Ontario illustrates the geographic distribution of six behavioural risk factors, by sex and age groups, for neighbourhoods across the province.
Through this atlas, public health in Ontario is empowered with local data to better understand the health of their communities. This information can help support the development of tailored prevention efforts to improve health and reduce local health disparities.
About Cancer Care Ontario
CCO is the Ontario government’s principal advisor on the cancer and kidney care systems, as well as on access to care for key health services. Encompassing Cancer Care Ontario and the Ontario Renal Network, CCO drives continuous improvement in disease prevention and screening, the delivery of care and the patient experience for chronic diseases. It provides tools, resources and evidence-based information to help its healthcare partners improve the delivery of care.
Estimating micro area behavioural risk factor prevalence from large population-based surveys: a full Bayesian approach
BMC Public Health
Abstract
Background: An important public health goal is to decrease the prevalence of key behavioural risk factors, such as tobacco use and obesity. Survey information is often available at the regional level, but heterogeneity within large geographic regions cannot be assessed. Advanced spatial analysis techniques are demonstrated to produce sensible micro area estimates of behavioural risk factors that enable identification of areas with high prevalence.
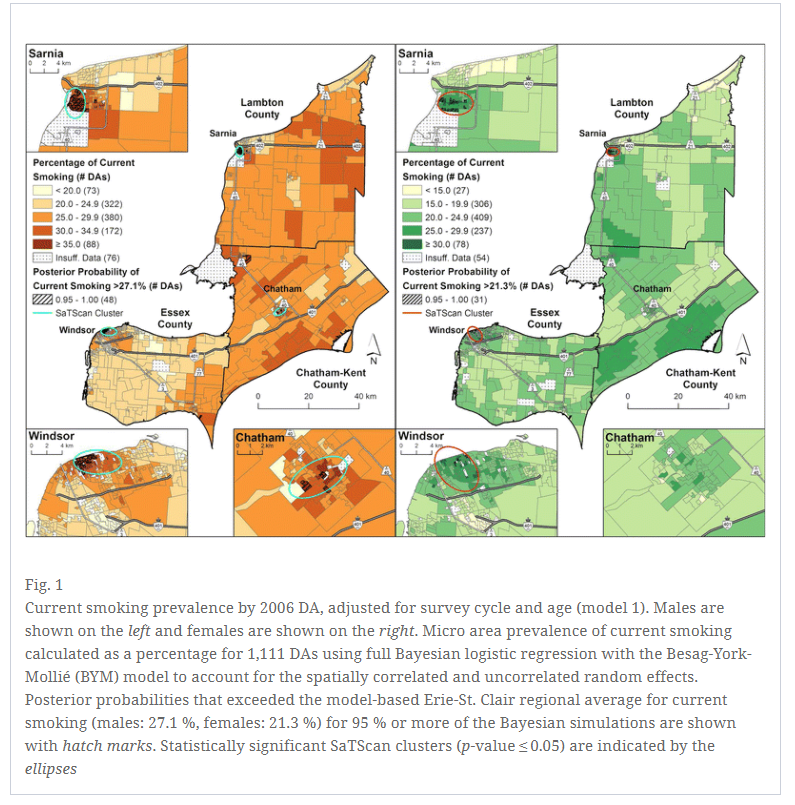
Methods: A spatial Bayesian hierarchical model was used to estimate the micro area prevalence of current smoking and excess bodyweight for the Erie-St. Clair region in southwestern Ontario. Estimates were mapped for male and female respondents of five cycles of the Canadian Community Health Survey (CCHS). The micro areas were 2006 Census Dissemination Areas, with an average population of 400–700 people. Two individual-level models were specified: one controlled for survey cycle and age group (model 1), and one controlled for survey cycle, age group and micro area median household income (model 2). Post-stratification was used to derive micro area behavioural risk factor estimates weighted to the population structure. SaTScan analyses were conducted on the granular, postal-code level CCHS data to corroborate findings of elevated prevalence.
Results: Current smoking was elevated in two urban areas for both sexes (Sarnia and Windsor), and an additional small community (Chatham) for males only. Areas of excess bodyweight were prevalent in an urban core (Windsor) among males, but not females. Precision of the posterior post-stratified current smoking estimates was improved in model 2, as indicated by narrower credible intervals and a lower coefficient of variation. For excess bodyweight, both models had similar precision. Aggregation of the micro area estimates to CCHS design-based estimates validated the findings.
Conclusions: This is among the first studies to apply a full Bayesian model to complex sample survey data to identify micro areas with variation in risk factor prevalence, accounting for spatial correlation and other covariates. Application of micro area analysis techniques helps define areas for public health planning, and may be informative to surveillance and research modeling of relevant chronic disease outcomes.
The opinions expressed in this article are those of the authors and may not represent the official positions of NAACCR.




 Every two and a half minutes someone in the United States will be diagnosed with lung cancer, with an estimated 234,030 new cases in the United States this year. The American Lung Association’s inaugural LUNG FORCE “State of Lung Cancer” 2018 report is the first time that these national and state lung cancer statistics have been analyzed in one report to show how the toll of lung cancer varies across the country and how every state and the nation can do more to protect residents from lung cancer.
Every two and a half minutes someone in the United States will be diagnosed with lung cancer, with an estimated 234,030 new cases in the United States this year. The American Lung Association’s inaugural LUNG FORCE “State of Lung Cancer” 2018 report is the first time that these national and state lung cancer statistics have been analyzed in one report to show how the toll of lung cancer varies across the country and how every state and the nation can do more to protect residents from lung cancer.
 The California legislature has enacted a regulation for all cancer service providers to provide electronic reporting to the Cancer Registry. This is expected to significantly increase the number of organisations supplying reports causing a concomitant enlarged volume of reports received annually. Furthermore across the USA there is an ageing CTR workforce without sufficient attraction of younger staff to sustain workforce numbers. This is further compounded by the ageing population who will also add to the increase of the total volume of cancer cases reported annually.
The California legislature has enacted a regulation for all cancer service providers to provide electronic reporting to the Cancer Registry. This is expected to significantly increase the number of organisations supplying reports causing a concomitant enlarged volume of reports received annually. Furthermore across the USA there is an ageing CTR workforce without sufficient attraction of younger staff to sustain workforce numbers. This is further compounded by the ageing population who will also add to the increase of the total volume of cancer cases reported annually.





